Understand Your Gut Microbiome with the Experts in GA
What are Microbiome and Probiotics?
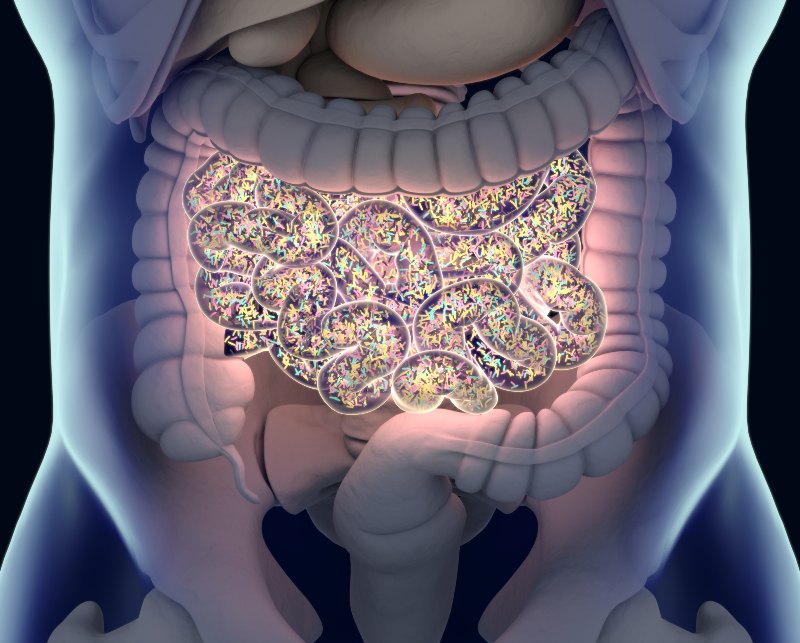
The microbiome refers to trillions of microorganisms residing in your gut, including bacteria, viruses, fungi, and other microbes. This diverse ecosystem plays a pivotal role in your overall health, influencing digestion, immunity, and even mental well-being.
Probiotics, on the other hand, are live beneficial bacteria or yeasts that you can consume through certain foods and supplements. These friendly bacteria are essential in supporting a balanced gut microbiome. Probiotics offer numerous benefits for digestive health and the rest of your body.
The Role of the Microbiome
Your gut microbiome is an incredibly dynamic environment that influences your digestive health significantly. It helps break down food, absorb nutrients, and produce essential vitamins. A healthy microbiome acts as a barrier against harmful bacteria and pathogens, reducing the risk of infections. It also communicates with the immune system, ensuring your body responds appropriately to potential threats.
Disruptions to the microbiome can lead to gut microbiome diseases such as inflammatory bowel disease (IBD), irritable bowel syndrome (IBS), and other digestive issues. Therefore, understanding what gut microbiome is and maintaining its balance is vital for good health. Our GI services can help you with this.
Benefits of Probiotics
Probiotics offer many health benefits by enhancing the composition of your gut microbiome. Some key probiotic health benefits include:
- Improved Digestion – Probiotics aid in breaking down food more efficiently, alleviating symptoms like bloating and constipation.
- Enhanced Immune Function – By promoting the growth of beneficial bacteria, probiotics support your immune system's ability to fight infections.
- Alleviation of GI Disorders – Studies have shown that probiotics can help manage symptoms of IBS and reduce the severity of IBD flare-ups.
- Better Mental Health – The gut-brain axis indicates that a healthy gut microbiome can positively impact mood and cognitive functions.
Sources of Probiotics
Probiotics can be found in various foods and supplements. Fermented foods are particularly rich in these beneficial bacteria. Some excellent sources include:
- Yogurt – A well-known probiotic-rich food that can improve gut health.
- Kefir – A fermented milk drink packed with diverse probiotic strains.
- Sauerkraut and Kimchi – Fermented vegetables that offer a robust mix of probiotics and fiber.
- Miso and Tempeh – Fermented soy products that are not only rich in probiotics but also protein.
- Probiotic Supplements – Available in pill, powder, or liquid form, these supplements provide concentrated doses of beneficial bacteria.
How to Maintain a Healthy Microbiome
- Eat a Diverse Diet – Consuming a variety of fruits, vegetables, and whole grains ensures a wide range of nutrients that promote a healthy microbiome.
- Limit Antibiotics – While necessary at times, antibiotics can disrupt the balance of your gut bacteria, so they should be used judiciously.
- Stay Active – Regular physical activity can positively affect gut microbiome diversity.
- Manage Stress – Chronic stress can negatively impact your gut health, so incorporating stress-reducing activities can be beneficial.
- Stay Hydrated – Drinking plenty of water supports the mucosal lining of the intestines, promoting a healthy microbiome.
Why Choose GI Specialists of Georgia?
Contact Us Today in Atlanta, GA
If you are interested in learning more about how the gut microbiome and probiotics can benefit your digestive health, or if you're seeking effective gut microbiome disease treatment, reach out to GI Specialists of Georgia. Our experienced team is ready to guide you on your journey to better health.
Don't wait to take charge of your digestive health. Contact us today to schedule a consultation and discover how we can support your gut health, digestion & microbiome support needs. Your well-being is our priority, and we are dedicated to helping you achieve optimal digestive health.
Explore our services and take the first step toward a healthier you.
Overview
Chronic constipation is defined as infrequent bowel movements or difficult passage of stools that persists for several weeks or longer.
Constipation is generally described as having fewer than one bowel movement every 3 days.
Occasional constipation is very common which can occur with changes in diet, new medications or stress. Some people experience chronic constipation that can interfere with their ability to go about their daily tasks. Chronic constipation may also cause excessive straining to have a bowel movement and other signs and symptoms. Constipation may also be related to a condition called irritable bowel syndrome.
Treatment for chronic constipation depends in part on the underlying cause. However, in some cases, a cause is never found.
Learn More about Constipation
Signs and symptoms of chronic constipation include:
- Having fewer than 1 bowel movement every 3 days
- Having lumpy or hard stools that are difficult or painful to pass
- Feeling as though there’s a blockage in your rectum that prevents bowel movements
- Feeling as though you can’t completely empty the stool from your rectum
- Needing help to empty your rectum, such as using your hands to press on your abdomen and using a finger to remove stool from your rectum
Blockages in the Colon or Rectum
Blockages in the colon or rectum may slow or stop stool movement. Causes include:
- Anal fissure
- Bowel obstruction
- Colon cancer
- Narrowing of the colon
- Other abdominal cancer that presses on the colon
- Rectal cancer
- Rectum bulge through the back wall of the vagina (rectocele)
Neurologic Conditions
Neurological problems can affect the nerves that cause muscles in the colon and rectum to contract and move stool through the intestines. Causes include:
- Autonomic neuropathy
- Multiple sclerosis
- Parkinson’s disease
- Spinal cord injury
- Stroke
Difficulty with the Muscles Involved in Elimination
Problems with the pelvic muscles involved in having a bowel movement may cause chronic constipation. These problems may include:
- Inability to relax the pelvic muscles to allow for a bowel movement (anismus)
- Pelvic muscles don’t coordinate relaxation and contraction correctly (dyssynergia)
- Weakened pelvic muscles
Factors that may increase your risk of chronic constipation include:
- Being an older adult
- Being a woman
- Being dehydrated
- Eating a diet that’s low in fiber
- Getting little or no physical activity
- Taking certain medications, including sedatives, narcotics, some
- antidepressants or medications to lower blood pressure
- Diabetes
- Pregnancy
- Low thyroid
Complications of chronic constipation include:
- Swollen veins in your anus (hemorrhoids). Straining to have a bowel movement may cause swelling in the veins in and around your anus.
- Torn skin in your anus (anal fissure). A large or hard stool can cause tiny tears in the anus.
- Stool that can’t be expelled (fecal impaction). Chronic constipation may cause an accumulation of hardened stool that gets stuck in your rectum causing significant discomfort.
- Intestine that protrudes from the anus (rectal prolapse). Straining to have a bowel movement can cause a small amount of the rectum to stretch and protrude from the anus.
- The following can help you avoid developing chronic constipation.
- Include plenty of high-fiber foods in your diet, including beans, vegetables, fruits, whole grain cereals, and bran.
- Eat fewer foods with low amounts of fiber such as processed foods, and dairy and meat products.
- Drink plenty of fluids.
- Stay as active as possible and try to get regular exercise.
- Try to manage stress.
- Don’t ignore the urge to pass stool.
- Try to create a regular schedule for bowel movements, especially after a meal.
Treatment for chronic constipation usually begins with diet and lifestyle changes meant to increase the speed at which stool moves through your intestines as described in prevention strategies above. If those changes don’t help, your doctor may recommend medications or surgery. Please see a physician, prior to self-treating this condition to avoid missing a serious or life-threatening condition.
Over the Counter Laxatives
Several types of laxatives exist. Each works somewhat differently to make it easier to have a bowel movement. The following are available over the counter:
- Fiber supplements. Fiber supplements add bulk to your stool. These include psyllium (Metamucil, Konsyl), calcium polycarbophil (FiberCon) and methylcellulose fiber (Citrucel).
- Stimulants including Correctol, bisacodyl (Ducodyl), Dulcolax and senna-sennosides oral (Senokot) cause your intestines to contract.
- Osmotic laxatives help fluids move through the colon. Examples include oral magnesium hydroxide (Phillips Milk of Magnesia), magnesium citrate, polyethylene glycol (Miralax).
- Lubricants such as mineral oil enable stool to move through your colon more easily.
- Stool softeners. Stool softeners such as docusate sodium (Colace) and docusate calcium (Surfak) moisten the stool by drawing water from the intestines.
- Enemas and suppositories. Sodium phosphate (Fleet), soapsuds or tap water enemas can be useful to soften stool and produce a bowel movement. Glycerin or bisacodyl suppositories also can soften stool.
Prescription Medications
If over-the-counter medications don’t help your chronic constipation, your doctor may recommend a prescription medication:
- Polyethelene glycol (PEG) (Golytely, Nulytely) and lactulose are available by prescription.
- Medications that draw water into your intestines. A number of prescription medications are available to treat chronic constipation. Lubiprostone (Amitiza) and linaclotide (Linzess), work by drawing water into your intestines and speeding up the movement of stool.
Training Your Pelvic Muscles
Biofeedback training involves working with a therapist who uses devices to help you learn to relax and tighten the muscles in your pelvis. Relaxing your pelvic floor muscles at the right time during defecation can help you pass stool more easily.
Surgery
Surgery may be an option if you have tried other treatments and your chronic constipation is caused by a blockage, rectocele, anal fissure or stricture.
For people who have tried other treatments without success and who have abnormally slow movement of stool through the colon, surgical removal of part of the colon may be an option. Surgery to remove the entire colon is rarely necessary.
Schedule an Appointment with Our Atlanta-Area Gastroenterologists
"*" indicates required fields

